Data extracted in July 2019.
Planned article update: April 2020.
Highlights
Among the EU Member States, France, Germany and Sweden had the highest healthcare expenditure relative to GDP in 2016 (11.0-11.5 %).
Current healthcare expenditure relative to GDP, 2016
This article presents key statistics on expenditure and financing aspects of healthcare in the European Union (EU). Healthcare systems are organised and financed in different ways across the EU Member States, but universal access to quality healthcare, at an affordable cost to both individuals and society at large, is widely regarded as a basic need; moreover, this is one of the common values and principles in EU health systems.
Statistics on healthcare expenditure and financing may be used to evaluate how a healthcare system responds to the challenge of universal access to quality healthcare, through measuring financial resources within the healthcare sector and the allocation of these resources between healthcare activities (for example, preventive and curative care) or groups of healthcare providers (for example, hospitals and ambulatory centres).
This article forms part of an online publication on Health in the European Union.
Health care expenditure
France, Germany and Sweden had the highest current healthcare expenditure relative to GDP in 2016 among the EU Member States
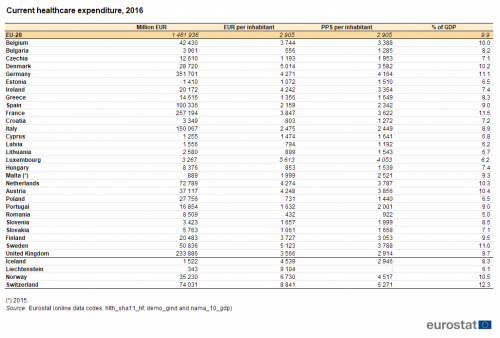
The level of current healthcare expenditure in Germany was EUR 352 billion in 2016 — the highest value among the EU Member States. France recorded the second highest level of current healthcare expenditure (EUR 257 billion), followed by the United Kingdom (EUR 234 billion).
Current healthcare expenditure in France was equivalent to 11.5 % of gross domestic product (GDP), more than in any other EU Member State — see Table 1. The next highest ratios were in Germany (11.1 %) and Sweden (11.0 %). Note that current healthcare expenditure in Switzerland was equivalent to 12.3 % of GDP, higher than the ratio in France. By contrast, current healthcare expenditure accounted for less than 7.5 % of GDP in 12 Member States, with Romania recording the lowest ratio (5.0 %).
Source: Eurostat (hlth_sha11_hf), (demo_gind) and (nama_10_gdp)
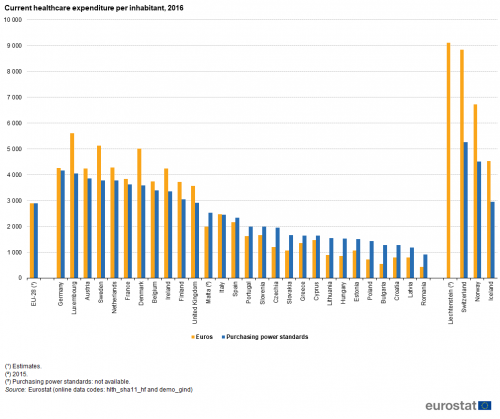
Relative to population size and in euro terms, current healthcare expenditure was highest among the EU Member States in Luxembourg (EUR 5.6 thousand per inhabitant), Sweden (EUR 5.1 thousand per inhabitant) and Denmark (EUR 5.0 thousand per inhabitant) in 2016. It is interesting to note that Luxembourg had the highest per capita ratio given that it had the second lowest ratio of healthcare expenditure to GDP, reflecting the high level of GDP in Luxembourg. Three of the EFTA countries included in Table 1 — Liechtenstein, Switzerland and Norway — each reported higher levels of healthcare expenditure per inhabitant than in any of the Member States. Following on from Luxembourg, Sweden and Denmark, a group of four Member States — the Netherlands, Germany, Austria and Ireland — recorded current healthcare expenditure around EUR 4.2-4.3 thousand per inhabitant. In turn, these were followed at some distance by another group — France, Belgium, Finland and the United Kingdom — with ratios in the range of EUR 3.6-3.8 thousand per inhabitant. There was then a relatively large gap to Italy (EUR 2.5 thousand per inhabitant), Spain (EUR 2.2 thousand) and Malta (EUR 2.0 thousand). All of the remaining Member States recorded average expenditure below EUR 1.7 thousand per inhabitant in 2016, with 7 of these 14 recording an average spend on healthcare below EUR 1.0 thousand per inhabitant. The lowest levels of average expenditure per inhabitant were in Bulgaria (EUR 556) and Romania (EUR 432). As such, the ratio between the highest (Luxembourg) and lowest (Romania) levels of expenditure per inhabitant was 13.0 : 1.
Source: Eurostat (hlth_sha11_hf) and (demo_gind)
These disparities were less when expenditure was expressed in purchasing power standards (PPS); this adjusts for differences in price levels between the EU Member States. Germany (4.2 thousand PPS per inhabitant), Luxembourg (4.1 thousand PPS per inhabitant), Austria (3.9 thousand PPS per inhabitant), Sweden and the Netherlands (both 3.8 thousand per inhabitant) recorded the highest ratios of healthcare expenditure per inhabitant in PPS terms. Romania (0.9 thousand PPS per inhabitant) had the lowest ratio and was the only EU Member State to report healthcare expenditure below 1.0 thousand PPS per inhabitant. As such, by taking account of price level differences, the ratio between the highest (Germany) and lowest (Romania) levels of healthcare expenditure per inhabitant was considerably narrower than the equivalent ratio in euro terms mentioned above, as it was 4.5 : 1.
Developments over time
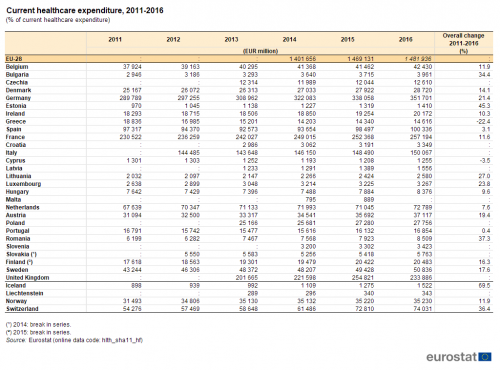
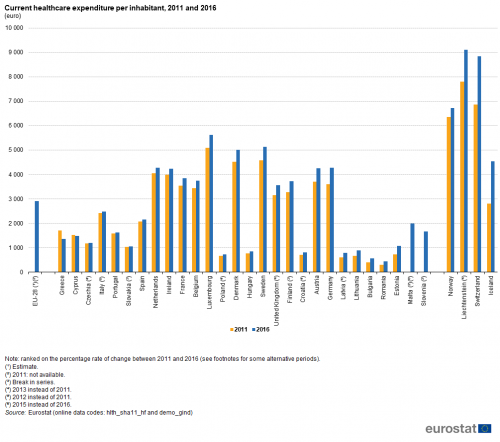
Table 2 and Figures 2 and 3 highlight the developments in the level of healthcare expenditure in recent years, focusing on a comparison between 2011 and 2016. Note that the analyses are presented in current price terms and so reflect price changes (inflation and deflation) as well as real changes in expenditure.
Among the 19 EU Member States for which 2011 and 2016 data are available, all except Greece and Cyprus recorded higher healthcare expenditure in 2016 than in 2011. The largest overall increase was observed in Estonia, where expenditure in 2016 was 45.3 % higher than in 2011, an increase equivalent to an average of 7.8 % per year. Among the three EFTA countries for which data are available, Iceland recorded an even larger increase, up 69.5 %, an average increase of 11.1 % per year. As well as Estonia, five other EU Member States — Romania, Bulgaria, Lithuania, Luxembourg and Germany — recorded overall increases of more than 20 %.
(% of current healthcare expenditure)
Source: Eurostat (hlth_sha11_hf)
As well as being affected by price changes, comparisons of healthcare expenditure over time can also be influenced by demographic changes. Figure 2 shows the average healthcare expenditure per inhabitant in 2011 and 2016 (see footnotes where alternative years have been used). Among the 26 Member States for which data are shown for two years (no older data available for Malta or Slovenia), Greece and Cyprus were again the only ones to record a lower expenditure in 2016 than in 2011. Equally, Estonia again recorded the largest increase, with average expenditure per inhabitant increasing by 46.6 %. As for the overall increase in expenditure, Romania (up 40.4 %), Bulgaria (38.6 %) and Lithuania (34.1 %) also recorded large increases in expenditure per inhabitant, as did Latvia (29.7 %, between 2013 and 2016). By contrast, the 23.8 % overall increase in healthcare expenditure in Luxembourg translated into a 10.3 % increase in expenditure per inhabitant, reflecting its relatively rapid population increase.
(euro)
Source: Eurostat (hlth_sha11_hf) and (demo_gind)
Figure 3 provides another analysis of the change in overall healthcare expenditure between 2011 and 2016, focusing on the ratio between this expenditure and GDP. Healthcare expenditure and GDP are both influenced by price changes and so, when combining the two indicators in a ratio, the impact of inflation may be cancelled out to some degree: this depends on the extent to which the price changes related to healthcare expenditure are similar to those experienced for the economy as a whole.
Nine of the EU Member States (no older data available for Malta or Slovenia) reported a lower ratio of healthcare expenditure to GDP in 2016 than in 2011 (2012 or 2013 for some Member States), three reported the same value for the ratio in both years, and 14 reported a higher ratio in 2016. By far the largest fall was in Ireland, where the ratio was 3.3 percentage points lower in 2016 (7.4 %) than it had been in 2011 (10.7 %). In the Member States where the ratio was higher in 2016 than it had been in 2011, the increase was generally 0.5 percentage points or less: Estonia (up 0.7 percentage points), Latvia (0.8 percentage points between 2013 and 2016) and Bulgaria (1.1 percentage points) recorded larger increases, as did Switzerland (1.5 percentage points) and Norway (1.7 percentage points) among the EFTA countries.

(%)
Source: Eurostat (hlth_sha11_hf) and (nama_10_gdp)
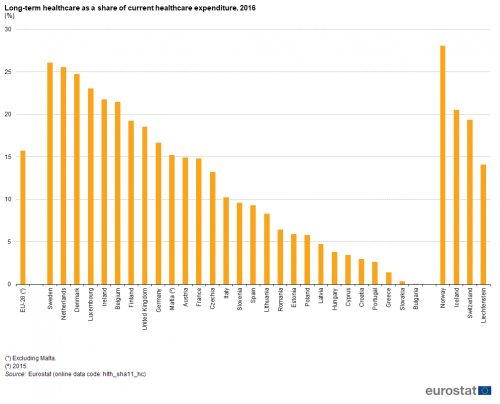
Overview of healthcare financing, functions and providers
Healthcare expenditure can be analysed from three perspectives: the sources of financing; the healthcare functions that are financed; the providers of healthcare.
Table 3 identifies the largest sources of financing, functions and providers (note that data for the EU-28 exclude Malta). Government schemes provided the financing for 36.7 % of all healthcare expenditure in the EU-28 in 2016, while compulsory contributory health insurance schemes and compulsory medical saving accounts accounted for 42.7 %. As such, these two sources accounted for 79.4 % of all financing. More than half (54.3 %) of healthcare expenditure in the EU-28 in 2016 was for curative and rehabilitative care, while nearly one fifth (18.4 %) was for medical goods. Hospitals were the largest providers of healthcare in expenditure terms, accounting for close to two fifths (37.4 %) of all expenditure in the EU-28. Providers of ambulatory health care (25.4 %) and retailers and other providers of medical goods (17.0 %) were the second and third largest providers in expenditure terms.
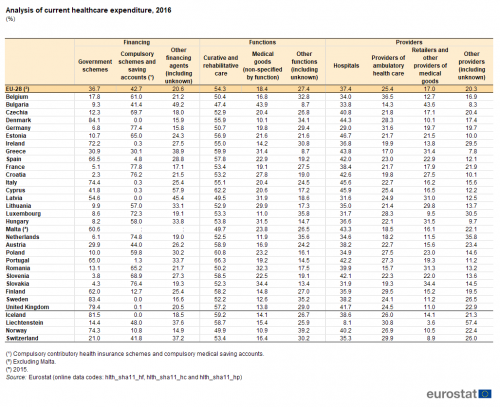
(%)
Source: Eurostat (hlth_sha11_hf), (hlth_sha11_hc) and (hlth_sha11_hp)
Table 4 shows how the expenditure for each of the largest sources of financing, functions and providers changed between 2011 and 2016. Data are available for 19 EU Member States. Between 2011 and 2016, the largest increase in financing in eight EU Member States (for example, in Belgium) was from government schemes while in four more (for example, in Portugal) it was from compulsory schemes and saving accounts; consequently there were seven Member States (for example, Lithuania) where expenditure from other financing agents increased more than from these two large sources.
In terms of the functions, in six EU Member States (for example, in the Netherlands) the largest increase was for expenditure on curative and rehabilitative care, while in four others (for example, in Bulgaria) expenditure increased most for medical goods. As such, in nearly half of the Member States for which data are available (9 out of 19; for example, in Luxembourg), the increase in expenditure on other functions was greater than for curative and rehabilitative care or for medical goods.
For the providers, the largest increase in expenditure between 2011 and 2016 in three EU Member States (for example, in Ireland) was for hospitals, while in seven more (for example, in Belgium) it was for providers of ambulatory health care and in four (for example, in Cyprus) it was for retailers and other providers of medical goods; consequently there were four Member States (for example, Estonia) where expenditure for other providers increased more than for these three large providers.
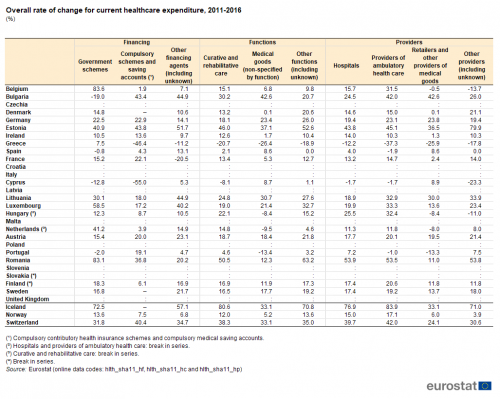
(%)
Source: Eurostat (hlth_sha11_hf), (hlth_sha11_hc) and (hlth_sha11_hp)
While Tables 3 and 4 offered an overview of the three perspectives (sources of financing, functions and providers), the remainder of the article looks at each of these perspectives in more detail.
Healthcare expenditure by financing scheme
Compulsory schemes and accounts financed more than half of healthcare expenditure in 14 EU Member States in 2016
Figure 4 provides a simplified analysis of healthcare expenditure by financing scheme, distinguishing: government schemes, compulsory contributory health care financing schemes and compulsory medical savings accounts (which are generally part of the social security system and are hereafter referred to as compulsory schemes/accounts), as well as all other financing schemes. The share of government schemes and compulsory schemes/accounts in total current healthcare expenditure was in excess of 80.0 % in Germany (where the highest share was recorded, at 84.2 %), Denmark, Sweden, France, Czechia, the Netherlands, Luxembourg and Slovakia; it was also above 80.0 % in Norway (which reported a share that was above that registered in any of the EU Member States, at 85.1 %) and Iceland among the EFTA countries.
With the exception of Cyprus, the combined expenditure from government schemes and compulsory schemes/accounts in 2016 exceeded the expenditure from all other sources in all of the EU Member States (2015 data for Malta) and all of the EFTA countries.
In most of the EU Member States, either government schemes or compulsory schemes/accounts dominated: in 10 Member States government schemes accounted for more than half of all expenditure and in 14 Member States compulsory schemes/accounts accounted for more than half of all expenditure. In Austria, compulsory schemes/accounts registered a larger share than government schemes or other sources, but less than half of the total. In the remaining three Member States — Bulgaria, Greece and Cyprus — other sources provided a larger share of financing than government schemes or compulsory schemes/accounts; only in Cyprus did other sources provide a majority (57.9 %) of the financing.
Compulsory schemes/accounts accounted for three quarters or more of overall spending on healthcare in France (77.8 %), Germany (77.4 %), Slovakia (76.4 %) and Croatia (76.2 %) in 2016, but less than 5.0 % in Spain, Portugal, Cyprus, Ireland, Italy, the United Kingdom, Denmark, Latvia and Sweden. By contrast, Denmark (84.1 %), Sweden (83.4 %) and the United Kingdom (79.4 %) reported that government schemes accounted for more than three quarters of their expenditure on healthcare, while shares of 65.0-75.0 % were registered in Italy, Ireland, Spain and Portugal.
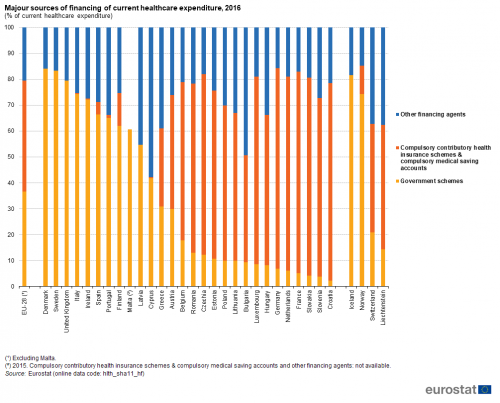
(% of current healthcare expenditure)
Source: Eurostat (hlth_sha11_hf)
Table 5 provides a similar analysis of healthcare expenditure by financing scheme, but with more detail concerning other financing schemes.
The third largest source of healthcare funding was household out-of-pocket payments, whose share average 15.7 % in the EU-28 (excluding Malta) in 2016. This share exceeded 40.0 % of the total in Latvia, Cyprus and Bulgaria (where it peaked at 48.0 %), while household out-of-pocket payments also accounted for more than one third of total healthcare expenditure in Malta and Greece. France was the only EU Member State where household out-of-pocket payments accounted for less than one tenth (9.8 %) of healthcare expenditure.
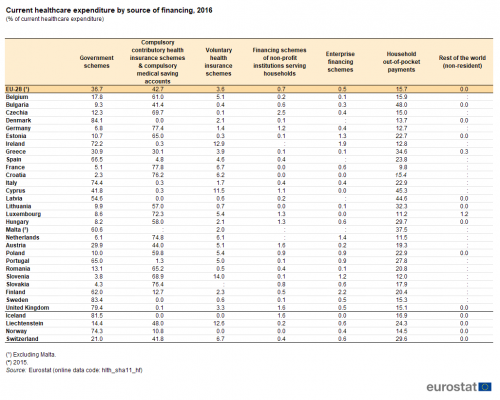
(% of current healthcare expenditure)
Source: Eurostat (hlth_sha11_hf)
Voluntary health insurance schemes generally represented a small share of healthcare financing among the EU Member States in 2016, averaging 3.6 % (excluding Malta). Their relative share peaked at 14.0 % in Slovenia, while shares above one tenth were also recorded in Ireland and Cyprus. The shares in these three Member States were clearly greater than elsewhere, as the next highest share was 6.7 % (in France). There were seven Member States where voluntary health insurance schemes provided less than 1.0 % of the finance for healthcare expenditure in 2016, with the lowest share recorded in Czechia (0.1 %).
The final analysis concerning financing (see Figure 5), shows the same sources of financing as in Table 5, but presented as values per inhabitant (in PPS) rather than as a share of all healthcare expenditure. This analysis shows how much on average is spent per inhabitant from each of the different sources. The total for all sources (the overall height of each stacked bar) shows the overall expenditure per inhabitant. To put this in perspective, the Member States and EFTA countries have been ranked based on the overall level of current healthcare expenditure relative to GDP.

(PPS per inhabitant)
Source: Eurostat (hlth_sha11_hf)
Healthcare expenditure by function
Curative and rehabilitative care services accounted for more than half of current healthcare expenditure in all except for three of the EU Member States
The functional patterns of healthcare expenditure presented in Figure 6 and Table 6 show that in 2016 curative and rehabilitative care services incurred more than 50.0 % of current healthcare expenditure in the vast majority of EU Member States, the exceptions being Malta (2015 data), Latvia and Bulgaria where the shares ranged from 47.4 % to 49.7 %. By contrast, at the upper end of the range, close to two thirds (66.3 %) of current healthcare expenditure in 2016 was incurred by curative and rehabilitative care services in Portugal, while Cyprus and Poland recorded shares that were above 60.0 %, with Greece (59.9%) just below this level.
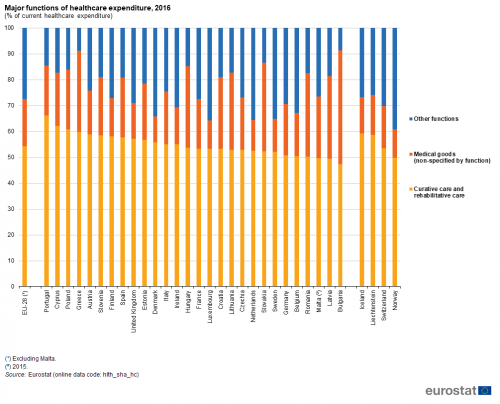
(% of current healthcare expenditure)
Source: Eurostat (hlth_sha_hc)
Medical goods accounted for just under one fifth of healthcare expenditure in 2016
Medical goods (non specified by function) were the second largest function in the EU-28 (excluding Malta), with an 18.4 % share of current healthcare expenditure. There was a substantial variation between the EU Member States in terms of the share of expenditure used for medical goods. The lowest shares — below 15.0 % — were recorded for Finland, Ireland, the United Kingdom, Sweden, the Netherlands, Luxembourg and Denmark (where the lowest share was recorded, at 10.1 %). By contrast, the highest shares — where medical goods accounted for 30.0-40.0 % of current healthcare expenditure in 2016 — were recorded for Greece, Hungary, Latvia, Romania and Slovakia, with this share peaking at 43.9 % in Bulgaria.
(% of current healthcare expenditure)
Source: Eurostat (hlth_sha11_hc)
The proportion of healthcare expenditure incurred by long-term healthcare was 15.7 % in the EU-28 (excluding Malta) in 2016: more information about this function is given in a special focus below.
The fourth largest function was ancillary services (such as laboratory testing or the transportation of patients), which accounted for 4.6 % of healthcare expenditure in the EU-28 (excluding Malta) in 2016. The share of these services exceeded 10.0 % in Cyprus and Estonia. Expenditure related to health system governance and the administration of financing averaged 3.6 % in the EU-28 (excluding Malta) and ranged from 0.8 % in Finland to 5.7 % in France. Expenditure for preventive care averaged 3.1 % of current healthcare expenditure in the EU-28 (excluding Malta), ranging from 1.2 % in Slovakia to 5.4 % in the United Kingdom.
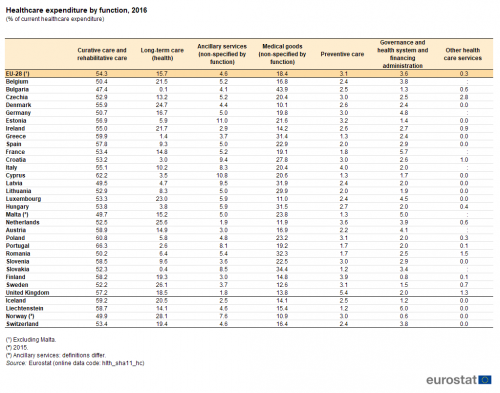
Focus on long-term healthcare expenditure
Long-term healthcare expenditure accounted for more than a quarter of current healthcare expenditure in Sweden in 2016
As noted above, services related to long-term healthcare (see Figure 7) accounted for 15.7 % of current healthcare expenditure in the EU-28 (excluding Malta) in 2016. The share was below 10.0 % in half of the EU Member States. Relatively low shares could be due to the main burden of long-term healthcare residing with family members, with no payment being made for providing these services. On the other hand, more than one fifth of healthcare expenditure was attributed to long-term healthcare in Belgium, Ireland, Luxembourg and Denmark, with this share reaching more than one quarter in the Netherlands (25.6 %) and Sweden (26.1 %); an even higher share (28.1 %) was recorded in Norway. It should be noted that it can be difficult to separate the medical and social components of expenditure for long-term care, leading to an inevitable impact on cross-country comparisons.
(%)
Source: Eurostat (hlth_sha11_hc)
Healthcare expenditure by provider
In expenditure terms, hospitals were the main provider of healthcare in most EU Member States
An analysis of current healthcare expenditure by provider is shown in Figure 8 and Table 7. It should be borne in mind that healthcare providers classified under the same group do not necessarily perform the same set of activities. For example, hospitals may offer day care, out-patient, ancillary or other types of service, in addition to in-patient services.
Hospitals accounted for the highest proportion (37.4 %) of healthcare expenditure in 2016 in the EU-28 (excluding Malta). Among the EU Member States, the share of current healthcare expenditure related to hospitals ranged from 29.0 % of the total in Germany to 46.7 % in Estonia. Three Member States reported that hospitals did not have the highest share of healthcare expenditure: ambulatory health care providers accounted for a greater share of total healthcare expenditure in Germany; retailers and other providers of medical goods accounted for a higher share in Bulgaria and Slovakia.
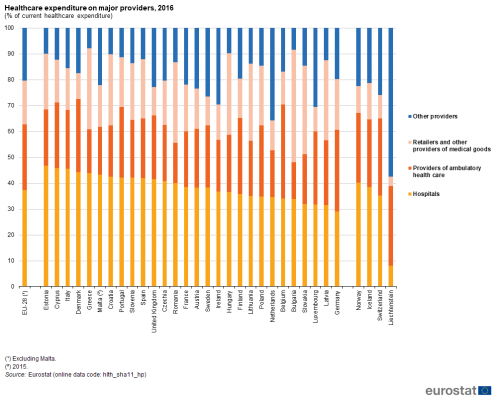
(% of current healthcare expenditure)
Source: Eurostat (hlth_sha11_hp)
The second largest healthcare provider (in expenditure terms) was generally that of ambulatory health care providers. Their share of current healthcare expenditure in 2016 averaged 25.4 % in the EU-28 (excluding Malta) and ranged from 14.3 % in Bulgaria to 31.6 % in Germany and 36.5 % in Belgium.
The share of current healthcare expenditure accounted for by retailers and other providers of medical goods averaged 17.0 % in the EU-28 (excluding Malta) in 2016. However, their share varied greatly between the EU Member State, from 9.5 % in Luxembourg to 34.4 % in Slovakia and 43.6 % in Bulgaria.
Table 7 gives information on the relative size of the providers shown in Figure 8 as well as more detailed information on the shares of other providers. By far the largest of the other providers was residential long-term care facilities, which accounted for 10.1 % of current healthcare expenditure in the EU-28 (excluding Malta) in 2016. Among the EU Member States, this share varied even more than the share for retailers and other providers of medical goods: the highest share for residential long-term care facilities was 25.8 % in the Netherlands, while in Croatia and Bulgaria the share was below 1.0 %.
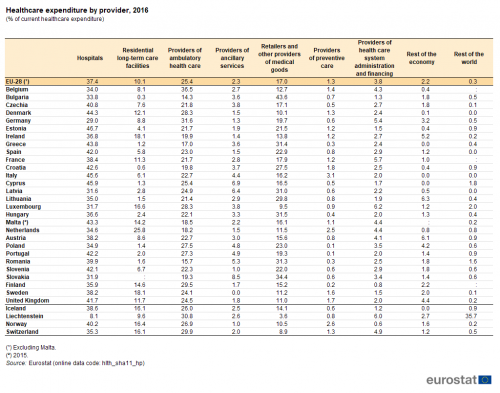
(% of current healthcare expenditure)
Source: Eurostat (hlth_sha11_hp)
Source data for tables and graphs
Data sources
Note on tables: — the symbol ‘:’ indicates that data are not available; — the symbol ‘–’ indicates that data are not relevant (for example a rate of change when the value for both periods is 0).
Key concepts
Current healthcare expenditure quantifies the economic resources dedicated to health functions, excluding capital investment. Healthcare expenditure is primarily concerned with healthcare goods and services that are consumed by resident units, irrespective of where that consumption takes place (it may be in the rest of the world) or who is paying for it. As such, exports of healthcare goods and services (to non-resident units) are excluded, whereas imports of healthcare goods and services for final use are included.
Long-term healthcare consists of a range of medical and personal care services that are consumed with the primary goal of alleviating pain and suffering and reducing or managing the deterioration in health status in patients with a degree of long-term dependency. The aim of long-term social care is to provide services and support, by formal and informal care givers, to individuals who, for reasons of disability, illness or other dependency, need help to live as normal a life as possible. Social care covers a wide range of services, including professional advice and support, accommodation, various types of assistance in carrying out daily tasks, home visits, home help services, provision of meals, special equipment, house adaptation for disabled persons, as well as assessment and care management services. There may be a mixed economy of health and social care provision and this mix of services can make it difficult to separate expenditure between health and social components. For the purpose of this article, the analysis of long-term care (as shown in Figure 7) is composed solely of the health component.
System of health accounts
Eurostat, the Organisation for Economic Cooperation and Development (OECD) and the World Health Organisation (WHO) established a common framework for a joint healthcare data collection exercise. The data collected relates to healthcare expenditure following the methodology of the system of health accounts (SHA).
The SHA shares the goals of the system of national accounts (SNA): to constitute an integrated system of comprehensive, internally consistent, and internationally comparable accounts, which should as far as possible be compatible with other aggregated economic and social statistical systems. Health accounts provide a description of the financial flows related to the consumption of healthcare goods and services from an expenditure perspective. Health accounts are used in two main ways: internationally, where the emphasis is on a selection of comparable expenditure data; nationally, with more detailed analyses of healthcare spending and a greater emphasis on comparisons over time.
In 2011, and as a result of four years of extensive and wide-reaching consultation, Eurostat, the OECD and the WHO released an updated manual for the collection of health accounts, ‘A system of health accounts, 2011 edition revised’. The core set of SHA tables addresses three basic questions: i) what kinds of healthcare goods and services are consumed; ii) which healthcare providers deliver them, and; iii) which financing schemes are used to deliver them?
Healthcare expenditure is recorded in relation to the international classification for health accounts (ICHA), defining:
- healthcare expenditure by financing schemes (ICHA-HF) — which classifies the types of financing arrangements through which people obtain health services; healthcare financing schemes include direct payments by households for services and goods and third-party financing arrangements;
- healthcare expenditure by function (ICHA-HC) — which details the split in healthcare expenditure following the purpose of healthcare activities — such as, curative care, rehabilitative care, long-term care, or preventive care;
- healthcare expenditure by provider (ICHA-HP) — which classifies units contributing to the provision of healthcare goods and services — such as hospitals, residential facilities, ambulatory health care services, ancillary services or retailers of medical goods.
Healthcare expenditure — methodology
Commission Regulation (EU) 2015/359 of 4 March 2015 implementing Regulation (EC) No 1338/2008 as regards statistics on healthcare expenditure and financing paves the way for healthcare expenditure data collection according to SHA 2011 methodology. The Regulation applies to data from reference year 2014 onwards and hence the information shown in this article presents a harmonised set of data based on this methodology.
Statistics on healthcare expenditure are documented in this background article which provides more information on the scope of the data, the legal framework, the methodology employed, as well as related concepts and definitions.
Context
Health systems across the globe are developing in response to a multitude of factors, including: new medical technology and improvements in knowledge; new health services and greater access to them; changes in health policies to address specific diseases and demographic developments; new organisational structures and more complex financing mechanisms. However, access to healthcare and greater patient choice is increasingly being considered against a background of financial sustainability. Many of the challenges facing governments across the EU were outlined in the European Commission’s White paper titled Together for health: a strategic approach for the EU 2008-2013 (COM(2007) 630 final), which built upon Council conclusions relating to Common values and principles in European Union Health Systems (2006/C 146/01).
In February 2013, the European Commission adopted a Communication titled Towards social investment for growth and cohesion (COM(2013) 83 final). Its main axes included: ensuring that social protection systems respond to people’s needs at critical moments throughout their lives; simplified and better targeted social policies, to provide adequate and sustainable social protection systems; and upgrading active inclusion strategies in the EU Member States.
In March 2014, the third multi-annual programme of EU action in the field of health for the period 2014-2020 was adopted (Regulation (EU) No 282/2014) under the title Health for Growth. This new programme emphasises the link between health and economic prosperity, as the health of individuals directly influences economic outcomes such as productivity, labour supply and human capital. A mid-term evaluation (COM(2017) 586 final) was published in October 2017. More information is provided in the introductory article for health statistics.
On the basis of Eurostat’s 2013 population projections (EUROPOP2013), long-run economic and budgetary projections aimed at assessing the impact of ageing population were published in 2015. This constituted the fifth release of such long-run projections since 2001. Taking account of underlying demographic and macro-economic assumptions and projections, age-related expenditures covering pensions, healthcare, long-term care, education and unemployment benefits were projected and analysed. These projections feed into a variety of policy debates in the EU, including the overarching Europe 2020 strategy. In particular, they are used in the context of the European semester so as to identify policy challenges, in the annual assessment of the sustainability of public finances carried out as part of the stability and growth pact. The next release of the long-run economic and budgetary projections is planned for spring 2018, with the underlying demographic and macro-economic assumptions and projections having already been published at the end of 2017.
In May 2016, the European Commission adopted a strategic plan for promoting health and food safety for the period 2016-2020. In order to improve the quality and effectiveness of public expenditure and contribute to prosperity and social cohesion, the European Commission seeks to provide expertise on health systems and support actions that help prevent and reduce the impact of ill-health on individuals and economies, while encouraging and supporting innovation and the uptake of modern technologies for better care delivery and cost-effectiveness.
The Directorate-General for Health and Food Safety has constituted a list of 88 European core health indicators (ECHIs) for monitoring progress in relation to health policy and broader Europe 2020 objectives. Among these, it recommends specifically following developments for:
Explore further
Other articles
Online publication
Methodology
General health statistics articles
Database
- Health (hlth), see:
- Health care (hlth_care)
- Health care expenditure (SHA 2011) (hlth_sha11)
Thematic section
Methodology
- Healthcare expenditure (SHA 2011) (ESMS metadata file — hlth_sha11_esms)
- A system of health accounts 2011 —revised edition March 2017
External links
- European Commission — Directorate-General for Health and Food Safety — European core health indicators (ECHI)
- European Commission — Directorate-General for Health and Food Safety — Health systems performance assessment
- European economy — The 2015 Ageing Report, Economic and budgetary projections for the 28 EU Member States (2013-2060)
- European economy — The 2015 Ageing Report, Underlying assumptions and projection methodologies
- European economy — The 2018 Ageing Report, Economic and budgetary projections for the 28 EU Member States (2016-2070)
- European economy — The 2018 Ageing Report, Underlying assumptions and projection methodologies
- OECD — Health at a Glance
- OECD — Health policies and data
- WHO Global health observatory (GHO)
- World Health Organisation (WHO) — Health systems
